Peripheral Vascular Disease In Lower Limb
PERIPHERAL VASCULAR DISEASE IN LOWER LIMB
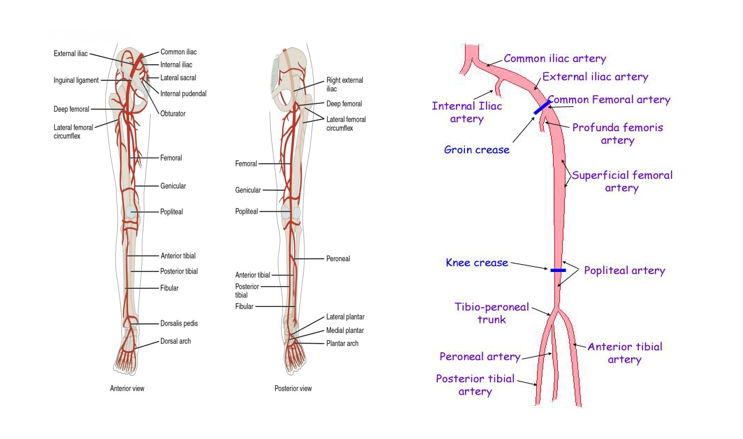
BRIEF ARTERIAL ANATOMY OF LOWER LIMB
Case 1
- Navin Shah 68/M
- Came with complaints of blackening over left little toe since 2 months
- He has been to 4 other hospitals where he could not get the satisfactory treatment and was advised lower limb amputation
- We have taken up the case and after discussions and meticulous planning with the help of available diagnostics and set off for the management
- H/o DM (Diabetes) / HTN (Hypertension) for the past 25 years
- H/o CAD-TVD (Coronary artery disease) on medical management
- H/o chronic smoking +
- Peripheral angiogram was done which showed ATA/PERONEAL ARTERY total occlusion, Distal Percutaneous Transluminal Angioplasty (PTA) 90% stenosis.
- He was first treated with POBA and angioplasty (Plain Old Balloon Angioplasty) to ATA / PTA and PERONEAL artery.
- Subsequently with limited amputation of just the little toe we are able to achieve our goal of limb salvage surgery.
Case 2
- T Rama Rao 61/m
- Came with complaints of ulcer over left foot for over 2 months. He is known case of heart disease undergoing treatment
- History of Diabetes since 25 years
- Evaluated – complete block of main artery supplying lower limb
- Treatment – PTA (Percutaneous Transluminal Angioplasty) with 3 stents
- Debridement and regular dressings has heeled the wound completely
Case 3
- Prathap Reddy 71/M
- k/c/o CAD (Coronary Artery Disease)
- History of HTN + (Hypertension) / DM + (Diabetes)
- C/o Blackish discoloration of left little toe
- Peripheral angiogram shows left ATA and PTA – 99% stenosis
- Treatment – Amputation of left 4th,5th toes followed by
BASICS
- In peripheral arterial disease there is a decreased or total loss of blood supply to the peripheries (most commonly affects lower limbs)
- Due to
- Embolism
- Atherosclerosis, thrombosis
- Trauma
- Complications of peripheral aneurysm
RISK FACTORS
- Age
- Gender – Male common
- Obesity
- Family history
- Diabetes
- Smoking
- Hypertension
- Dyslipidemia
- Hyperhomocysteinemia
- Race (Asian / Hispanic / black vs white)
STATISTICS
- Approximately 12% of the adult population has PAD, almost 20% of adults older than 70 years have PAD
- A new analysis published by THE SAGE GROUP concludes that atherosclerotic peripheral arterial disease (PAD) afflicts over 20 million in India
- Once PAD has progressed to CLI (Chronic Limb Ischemia), the risks of limb loss and mortality increase. At six months approximately 20% of those with CLI will die; another 40% will experience amputation.
- Diabetics represent 60% to 80% of CLI patients, we believe that India may unfortunately be on the path to becoming the Critical Limb Ischemia Capital
WHY MORE COVERAGE
- Under diagnosed, undertreated, and poorly understood even by the physicians and much more common than thought considering the lifestyle and the rise of share of the non communicable diseases like hypertension and diabetes.
- The diagnosis of PAD should not be overlooked for 2 important reasons. First, patients with PAD may experience many problems, such as claudication, ischemic rest pain, ischemic ulcerations, repeated hospitalizations, revascularizations, and limb loss. These lead to a poor quality of life and a high rate of depression
- Cardiovascular death and have a higher rate of all-cause mortality compared with patients without PAD.
TREATMENT EARLIER
- Amputation if wound does not heal and necrosis due to compromised blood supply revised amputation resulting in high morbidity and mortality rates
- Due to new modalities for diagnosis such as colour doppler, CT angio, DSA, MRA and new interventions like peripheral stenting with advanced stents
- Level of obstructed supply can be made and appropriate intervention can be done
HOW WE DO IT
- Depending on the stage of presentation
- Non healing ulcer – debridement if needed after endovascular technique
- Gangrene – Infected – Amputate to reduce sepsis – endovascular technique
- Non infected – endovascular technique – amputate
- Vasodilators to increase blood supply and anticoagulants and anti platelets for stent patency and anti diabetics, anti hyper lipidemics and anti hypertensives depending on the risk factors and regular dressings and wound care.
- The goals of therapy are to improve symptoms and thus quality of life and to decrease the cardiovascular event rate (myocardial infarction, stroke, cardiovascular death)
- Accomplished by establishing a
- Supervised exercise program and
- Administering cilostazol or performing a revascularization procedure if medical therapy is ineffective.
- A comprehensive program of cardiovascular risk modification (discontinuation of tobacco use and control of lipids, blood pressure, and diabetes) will help to prevent the latter
STENT
- Stent placement is typically used when residual stenosis after PTA is 30% or greater
- Primary stent placement has become a viable alternative for treating ulcerative lesions that may potentially be the source for embolization
- Several clinical studies have demonstrated the significant improvements of the new generation of nitinol stents for the SFA lesions: the German Multicenter Experience, the Mewissen trial, the BLASTER Trial, and the SIROCCO trial
TAKE HOME MESSAGE
Watch out for
- Tingling sensation in the legs
- Pain after walking a certain amount distance
- Sudden rest pain
- Ulcerations
- Blackening
- Especially on the background of the above said risk factors
- Better to get evaluated about the limb and the doctor will decide if your heart status also needs to get evaluated
MOTTOS
- Salvaging your precious limb
- Adding miles to your walk