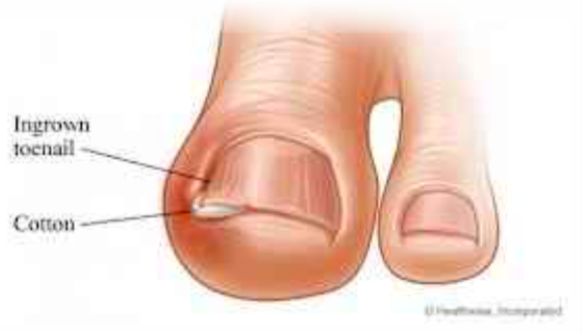
Ingrowing Toenails
One of the most common foot disorders is an ingrown toe nail. The edge of the nail grows into the skin at the side of the nail, and the area becomes infected. The skin is red and inflamed, and the toe hurts. Pus may form. Major factors which can cause the problem are:- Tight shoes
- Tight socks
- Cutting the nail too short with rounded edges
Treatment An ingrown toenail can often be effectively treated by antibiotics, surgical removal of a wedge of nail, avoiding tight shoes and tight socks and avoiding improper Post operation cutting of toenail. Post operation a bulky dressing will be applied to the A chronic ingrown toenail with recurrent infections may toe. This should not be removed for 7 days. You will not require surgery. be able to drive yourself. Please make arrangements for transport home in advance.
Surgery Please keep your foot elevated above the level of your heart as much as possible for 72 hours after surgery with a wedge resection of the nail, the surgeon removes this will reduce swelling and bleeding - both of which a strip of nail at the side and a small part of the nail bed. may increase the risks of local infection. The nail will then grow straight and not grow into the skin. You need to ensure that you have an appointment 7-10 days post-op so that the dressings may be reduced Usually one edge of the nail is removed. In some cases and any sutures removed both left and right edges are removed. To treat severe cases the surgeon may need to remove Complications the whole nail and the complete nail bed.
These include: The surgery is a day-case procedure.
- It may be Infection
- Performed under local anaesthetic or general
- Recurrence of ingrown nails anaesthetic
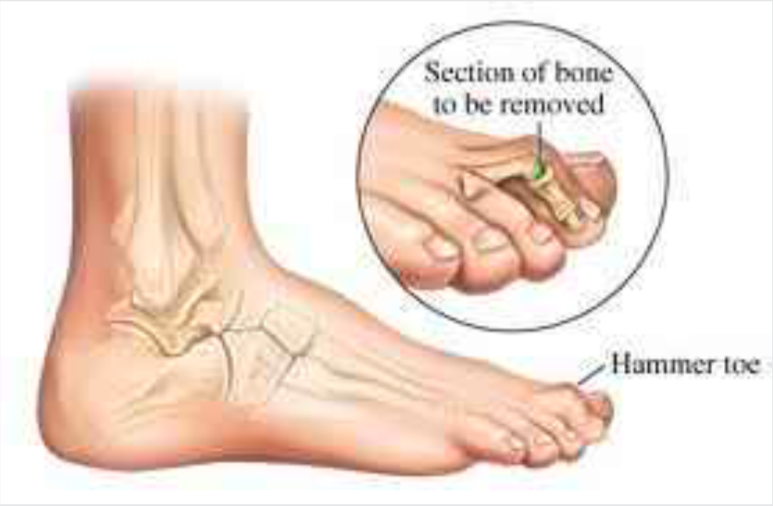
Hammer Toes and Corn
Complications include: Hammer Toes and Corns- Recurrence.
- Over Correction. Dr. Pradeep Moonot
- Orthopaedic Surgeon
- Infection at the site of the wound.
- Toe stiffness. Specialist in foot, ankle and knee surgery
- Nerve injury at the time of surgery
The Injury
Plantar Fasciitis (heel-spur syndrome) is a common problem. It starts as a dull intermittent pain in the heel which may progress to a sharp persistent pain. Classically, it is worse in the morning with the first few steps, after sitting, after standing or walking, and at the beginning of sporting activity. The plantar fascia is a thick fibrous material on the bottom of the foot. It is attached to the heel bone (calcaneus), fans forward towards the toe, and acts like a bowstring to maintain the arch in the foot. A problem may occur when part of this inflexible fascia is repeatedly placed under tension, as in running. Tension causes an overload that produces an inflammation usually at the point where the fascia is attached to the heel bone. The result is pain. Plantar fascia injury may also occur at midsole or near the toes. Since it is difficult to rest the foot, the problem gradually becomes worse because the condition is aggravated with every step. The inflammatory reaction at the heel bone may produce spike-like projections of new bone called heel-spurs. They are sometimes shown on X-rays. The exact relationship between heel spurs and plantar fasciitis is poorly understood. The heel spurs do not cause the heel pain and they are not the initial cause of the problem. Indeed some people may have heel spurs found incidentally on X-rays but may be completely pain free. Treatment : Improvement may take longer than expected, especially if the condition has been present for a long time. During recovery, loss of excess weight, good shoes and sedentary activities all help the injury to heal. You should return to full activity gradually. Rest: Use pain as your guide. If your foot is too painful, rest it. Ice: Ice the sore area for 30-60 minutes several times a day to reduce the inflammation. Apply a plastic bag of crushed ice over a towel. You should also ice the sore area for 15 minutes after activity. Medication: If your condition has developed recently, anti-inflammatory/ analgesic medication (in tablet form), coupled with heel pads may be all that is necessary to relieve pain and reduce inflammation. If no pain relief has occurred after two or three months, however, an injection of either cortisone and/ or local anaesthetic directly into the tender area may be considered. Physiotherapy: The initial objective of physiotherapy (when needed) is to decrease the inflammation. Later, the small muscles of the foot can be strengthened to support the weakened plantar fascia. Heel Pads: A heel pad of felt, sponge or a newer synthetic material can help to spread, equalize and absorb the shock as your heel lands, thus easing the pressure on the plantar fascia. Shoes: Poorly fitting shoes can cause plantar fasciitis. The best type of shoe to wear is a good running shoe (jogger/trainer) with excellent support. The shoe that fits best should be chosen. Experiment with your athletic shoes to find a pair that is comfortable and gives you fewer symptoms. Orthoses: Orthoses are shoe inserts that Dr. Pradeep Moonot may prescribe if necessary. Taping: Taping your foot to maintain the arch may benefit some people as this can take some of the pressure off the plantar fascia. Night Splints: These are plastic splints that keep the foot stretched and the ankle at right-angles when you are asleep. This maintains the tension in the plantar fascia and may help to alleviate some early morning symptoms during the first few steps of the day. Surgery: Surgery is rarely required for plantar fasciitis. It would be considered treatment if the pain is still incapacitating after at least 12 months of treatment. When needed, surgery involves release of the plantar fascia and release of a small nerve. Sports Plantar fascia can be aggravated by all weight bearing sports. Any sport where the foot lands repeatedly, such as jogging or running can aggravate the problem. To maintain cardiovascular fitness, weight bearing sports can be temporarily replaced by non weight bearing sports (like swimming, cycling). Weight training can be used to maintain leg strength. When recovering from plantar fasciitis, return to sports activities slowly. If you have a lot of pain either during the activity or the following morning, you are doing too much. Exercise Stretches: Stand at arms’ length from a counter or table with your back knee locked and your front knee bent. Slowly lean towards the table, pressing forward until a moderate stretch is felt in the calf muscles of your straight leg. Hold 10 seconds. Keeping both your heels on the floor, bend the knee of your straight leg until a moderate stretch is felt in your Achilles tendon. (Tendons attach muscles to bones; the Achilles tendon attaches the muscles of the calf to the heel bone). Hold 10 seconds. You should feel a moderate pull in your muscles and tendon, but no pain. Change legs and stretch the other leg. Repeat 10 times, 3 times a day.The Injury
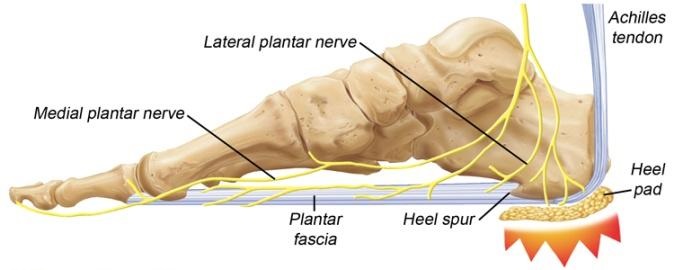
Plantar Fasciitis (heel-spur syndrome) is a common problem. It starts as a dull intermittent pain in the heel which may progress to a sharp persistent pain. Classically, it is worse in the morning with the first few steps, after sitting, after standing or walking, and at the beginning of sporting activity.
The plantar fascia is a thick fibrous material on the bottom of the foot. It is attached to the heel bone (calcaneus), fans forward towards the toe, and acts like a bowstring to maintain the arch in the foot.
A problem may occur when part of this inflexible fascia is repeatedly placed under tension, as in running. Tension causes an overload that produces an inflammation usually at the point where the fascia is attached to the heel bone. The result is pain. Plantar fascia injury may also occur at midsole or near the toes. Since it is difficult to rest the foot, the problem gradually becomes worse because the condition is aggravated with every step.
The inflammatory reaction at the heel bone may produce spike-like projections of new bone called heel-spurs. They are sometimes shown on X-rays. The exact relationship between heel spurs and plantar fasciitis is poorly understood. The heel spurs do not cause the heel pain and they are not the initial cause of the problem. Indeed some people may have heel spurs found incidentally on X-rays but may be completely pain free.
Treatment
Improvement may take longer than expected, especially if the condition has been present for a long time. During recovery, loss of excess weight, good shoes and sedentary activities all help the injury to heal. You should return to full activity gradually.
Rest: Use pain as your guide. If your foot is too painful, rest it.
Ice: Ice the sore area for 30-60 minutes several times a day to reduce the inflammation. Apply a plastic bag of crushed ice over a towel. You should also ice the sore area for 15 minutes after activity.
Medication: If your condition has developed recently, anti-inflammatory/ analgesic medication (in tablet form), coupled with heel pads may be all that is necessary to relieve pain and reduce inflammation. If no pain relief has occurred after two or three months, however, an injection of either cortisone and/ or local anaesthetic directly into the tender area may be considered.
Physiotherapy: The initial objective of physiotherapy (when needed) is to decrease the inflammation. Later, the small muscles of the foot can be strengthened to support the weakened plantar fascia.
Heel Pads: A heel pad of felt, sponge or a newer synthetic material can help to spread, equalize and absorb the shock as your heel lands, thus easing the pressure on the planter fascia.
Shoes: Poorly fitting shoes can cause plantar fasciitis. The best type of shoe to wear is a good running shoe (jogger/trainer) with excellent support. The shoe that fits best should be chosen. Experiment with your athletic shoes to find a pair that is comfortable and gives you fewer symptoms.
Orthoses: Orthoses are shoe inserts that Dr Pradeep Moonot may prescribe if necessary.
Taping: Taping your foot to maintain the arch may benefit some people as this can take some of the pressure off the plantar fascia.
Night Splints: These are plastic splints that keep the foot stretched and the ankle at right-angles when you are asleep. This maintains the tension in the plantar fascia and may help to alleviate some early morning symptoms during the first few steps of the day.
Surgery: Surgery is rarely required for plantar fasciitis. It would be considered treatment if the pain is still incapacitating after at least 12 months of treatment. When needed, surgery involves release of the plantar fascia and release of a small nerve.
Sports Plantar fascia can be aggravated by all weight bearing sports. Any sport where the foot lands repeatedly, such as jogging or running can aggravate the problem. To maintain cardiovascular fitness, weight bearing sports can be temporarily replaced by non weight bearing sports (like swimming, cycling). Weight training can be used to maintain leg strength. When recovering from plantar fasciitis, return to sports activities slowly. If you have a lot of pain either during the activity or the following morning, you are doing too much.
Exercise Stretches: Stand at arms’ length from a counter or table with your back knee locked and your front knee bent. Slowly lean towards the table, pressing forward until a moderate stretch is felt in the calf muscles of your straight leg. Hold 10 seconds. Keeping both your heels on the floor, bend the knee of your straight leg until a moderate stretch is felt in your Achilles tendon. (Tendons attach muscles to bones; the Achilles tendon attaches the muscles of the calf to the heel bone). Hold 10 seconds. You should feel a moderate pull in your muscles and tendon, but no pain. Change legs and stretch the other leg.
Repeat 10 times, 3 times a day.
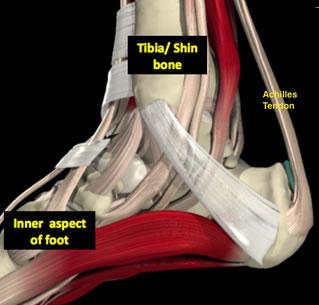
 What causes Achilles tendon pain?
What causes Achilles tendon pain?
- In many patients no definite cause is found.
- The Achilles tendon can withstand huge forces even in people who are recurrently stressing it, such as in long distance running however despite good conditioning, pain can ensue.
- Rapid increases or changes in training regimes can precipitate the symptoms.
- Inappropriate shoe-wear that can alter the mechanics of your foot when you hit the ground whilst running can increase symptoms.
- Patients with more general symptoms such as those associated with different types of arthritis/inflammatory disorders can develop Achilles pain.
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Swelling that is present all the time and can get worse throughout the day with activity
- Severe pain the day after exercising
- Thickening of the tendon
- Achilles tendon degeneration
- Bone spurs at the tendon insertion
Medical Team
DR. PRADEEP MONOOT
MBBS (Bom), MS (Ortho)(Bom), DNB (Orth), MRCS (UK), FRCS (Ortho) (UK)