Pain & Pain Management In Surgical / Trauma
What is pain?
Pain is an unpleasant physical and emotional response to actual or potential tissue damage or described in terms of such damage.
It is a protective response which ensures that an injured part of the body is carefully handled and further damage is prevented.
Why do we feel pain?
There are nerve endings distributed all over our body- from the skin to the intestines. These get activated in response to injuries from varied mechanisms like cuts and bruises, deep pressure, burns, extreme cold etc. Upon activation, signals are sent by the nerve endings to the brain and pain is perceived.
Why is it important to reduce pain?
Control of pain leads to a better life – Pain is unpleasant. It leads to emotional responses like depression and anger. It imposes a financial burden on the individual as well as society not only because of the expenses of treatment but also because there is loss of productive work-hours in the affected population. Long-lasting pain affects day-to-day functioning. People with pain tend to handle that body part carefully leading to stiffening of the joints and loss of muscle mass due to disuse. The stress leads to lack of control of blood pressure and blood sugar, sleeplessness, increase in acidity and body weight.
In patients undergoing surgery, pain relief leads to early recovery which means the patient walks sooner (Decreasing the chances of blood clots forming in the legs and travelling to the heart). He has better control of blood pressure and blood sugars due to decrease in stress levels and is less prone to stress-related complications like heart failure. All this leads to earlier discharge from the hospital.
How is pain classified?
There are various ways to classify pain:
There can be more than one type of pain in a patient due to more than one cause. This is important to know because the treatment changes with the cause/type/duration.
Based on the duration it can be acute i.e. immediate or sudden, usually lasting from 3 to 6 months or chronic i.e. long-lasting-more than 6 months or acute-on-chronic i.e. sudden pain superimposed upon a pre-existing pain. Pain can be mitigated by non invasive or invasive means. Non invasive methods include oral medicines (Aspirin, Paracetamol, Morphine etc.) Hot fomentation, cold compresses, physiotherapy, yoga and so on. Based on the site of origin it can be Somatic i.e. arising from the skin/bones/muscles or visceral i.e. from the internal organs like the intestine or uterus. Based on the cause of pain it can be Neuropathic i.e. arising from nerves which are injured or inflammatory i.e. due to chemicals released after injury.
What are the common means of reducing pain?
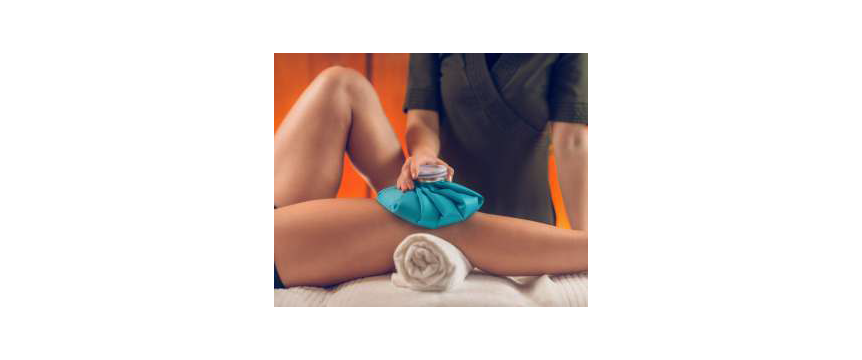
Pain can be mitigated by non invasive or invasive means. Non invasive methods include oral medicines (Aspirin, Paracetamol, Morphine etc.) Hot fomentation, cold compresses, physiotherapy, yoga and so on.
Invasive methods include pain killer injections either into the muscles or veins and more recently blocking nerves causing pain with anaesthetic drugs. Each method has its advantages and disadvantages.

Medicines which are called NSAIDS ( Nonsteroidal Anti- Inflammatory Drugs) include Ibuprofen and Diclofenac. They act by decreasing the inflammation at the site of the pain. But when taken for a prolonged duration they might cause damage to the kidneys. They should also not be taken by those suffering from asthma or heart/bleeding problems.
Opioid drugs like Morphine, while very very effective, are the leading cause of addiction in the US and active research is ongoing to find alternate means of pain relief especially in the acute setting of trauma or surgery.
My friend recently had an accident and fractured his thigh bone and has to undergo surgery. What modes of pain relief can she be given?
After an accident there are various factors to take into consideration before pain relief methods can be planned. The treatment differs for young people with no other health issues vis-a-vis older persons with say high blood pressure or diabetes or kidney failure. It will also change with the extent and region of injury, ensuing blood loss, ability of the patient to breathe adequately, neurological status (Drowsy/conscious) and the expertise of the medical personnel.
In all cases no one method is considered superior or enough by itself. A multi-prong approach to pain relief ranging from oral/IV medicines to blocking the nerves carrying pain from the injured area (nerve block) helps in lessening the side effects, complications and costs involved.
What is a nerve block?
A nerve block involves deposition of local anaesthetic drugs near a nerve or a bundle of nerves to temporarily stop them from working. This cuts off pain transmission at the very first step.
For example this patient with a fracture of the thigh bone will have severe pain upon any sort of movement and may be taken up for surgery only after a few days especially if she has other problems like being on blood-thinning medicines or uncontrolled diabetes. In the meantime she will need a femoral nerve block along with other pain medication. The femoral nerve is present on the front of the thigh near the groin.
How is the nerve block given?
Before giving the nerve block we ensure that the nerve itself is not injured from the accident by testing sensation and muscle movement. If there is any doubt we do not proceed with the block and give alternate means of pain relief.
Nerve blocks are given by qualified Anaesthesia doctors. All nerves in the body have more or less a constant location in humans. They can be identified by means of landmarks e.g. the femoral nerve is close to the major artery in the groin whose pulsations are easily felt.
Sometimes the Anaesthetist might use a needle through which very small current pulses are given in order to locate the nerve. These pulses do not cause pain and are felt more like vibrations. When the needle is close to the nerve, the muscles supplied by the nerve show contraction. With the femoral nerve the muscles on the front of the thigh will move. At this point all the drug is given.
Another precise way of identifying the nerve is by using ultrasound where the pulsating artery and the nerve next to it are visible on the screen.
After the drug is injected the patient will get pain relief in 5- 10 minutes. If prolonged pain relief needs to be given we leave small tubes called catheters next to the nerves and give a constant supply of the numbing medicine through syringe pumps for as long as needed (commonly 3-4 days).
Will I have pain when the nerve block is given?
No, the doctor will first give a small numbing injection on the skin before using the other needle.
How soon will I get pain relief and how much of relief can I expect? Is there a way to measure pain?
Pain relief usually starts within 10 minutes and depends on the concentration of the drug given. It might take upto an hour for maximum relief. The extent of relief varies from tolerable pain to sometimes complete relief.
The level of pain perceived is very individual-specific. Some people can bear the pain after hip replacements and some may cry holy murder while an IV cannula is being placed.
Most commonly the health care provider uses a Visual Analogue Scale (VAS) to note down the pain level being experienced. This is a scale where the facial expression of the patient is assigned a number ranging from 0 to 10 . Here 0 means a happy face and 10 denotes extreme crying. Similarly, the healthcare provider or nurse might ask the patient to give a number to the pain being experienced (numerical scale). Again 0 means no pain and 10 is the worst pain imaginable. The aim for us is usually to bring the pain down to less than 3 denoting mild/tolerable pain.
Will there be any side effects/complications of the nerve block?
Like any procedure done on the human body there are always chances of complications during nerve blocks. When done by expert hands minor complications are infrequent and major complications are rare.
These range from failed blocks with no pain relief, injury to blood vessels/lungs/nerves/other organs, temporary weakness of the muscles supplied by the nerve and very rarely injection of the drug into blood vessels leading to Local Anaesthetic Systemic Toxicity.
The doctors giving the nerve blocks are trained to prevent and recognise such complications. They will use full monitoring like blood pressure, ECG and oxygen saturation in the blood before, during and for 3 to 4 hours after the procedure. You will need to be admitted in the hospital for that duration.
Why should I undergo a nerve block when there are other means of pain relief ?
Different degrees of pain need different methods of treatment.
A simple headache after a sleepless night might subside after an oral painkiller. Pain due to falling on the ground while running might need an injection into your arm/buttock. A fracture pain or one after a surgery will need oral medicines, injectable painkillers like IV Morphine and yet not lead to adequate relief. It is such pain which benefits from nerve blocks. In the surgical setting physiotherapy and active movements become easier and less painful if continuous pain relief is given with nerve block catheters. Our patients undergoing total knee replacement generally walk within 4 hours of surgery.
Further most analgesics (painkillers) come with their own respective set of side effects. Many of them cannot be used if you have a history of poor kidney function/ asthma/ heart attacks/bleeding tendencies. They can lead to nausea, dizziness, retention of urine, constipation, breathing difficulty, drowsiness etc.
In the trauma/surgical setting we need to use all methods in order to attack every step of the pain pathway in the body and minimise the overall dose of individual drugs. So you will be getting oral medicines, IV injections as well as nerve blocks. These have an additive effect and individual doses of each medicine reduce drastically.
How long does pain last after surgery?
After any surgery maximum pain is felt during the first 3 to 4 days and this gradually decreases over a period of the next 7 days.
My father has fractured his ribs and finds it difficult to breathe without pain. He cannot afford to take long leave from work. Can nerve blocks help?
Yes, rib injuries prevent patients from taking deep breathes due to pain. This causes gradual collapse of the small airways in the lungs. The ensuing inadequacy of oxygen in the body and chances of developing pneumonia will require hospitalisation.
Such patients can be helped by the placement of Erector Spinae or Serratus Anterior plane blocks. A small catheter will be placed in between the muscles of the chest wall or back and a continuous infusion of local anaesthetic medicine will be given from a portable infusion pump which can be taken home. Deep breathing exercises are thus possible and prevent deterioration of the lung and loss of work-hours.
The infusion pumps will contain medicine for upto 48 hours and you will need to get it refilled at the hospital. A week of such treatment will give enough time for the body to heal.