Joint Replacement Summary
Update on Joint Replacement Surgery
Joint replacement surgery has come a long way over the last six decades. The most common joints that are being replaced across the world are the knee, hip, shoulder, elbow and ankle in that order. In the USA over 700,000 knee and around 400,000 hip replacements are done annually. These numbers are expected to rise exponentially to over 4 million procedures by 2030. The data in India is not very robust but estimates vary between 100,000 – 200,000 knee replacement procedures. Hip replacement numbers are substantially less. Indians seem genetically more predisposed to knee arthritis compared to their counterparts in the West. The most common indication for knee replacement is osteoarthritis. In contrast, Indians seem well protected against osteoarthritis of the hip which is very common in the West. The most common indication for a hip replacement in India is Avascular Necrosis because of injudicious and rampant use of steroids by medical practitioners.
Knee Replacement:
Indications for a knee replacement include :
- Osteoarthrtitis
- Rheumatoid arthrits
- Post traumatic arthritis
When is a knee replacement advisable? I generally advise surgery in patients who have advanced arthritis when conservative measures have failed to control the pain and disability. Age should not be a criterion for advising a knee replacement.
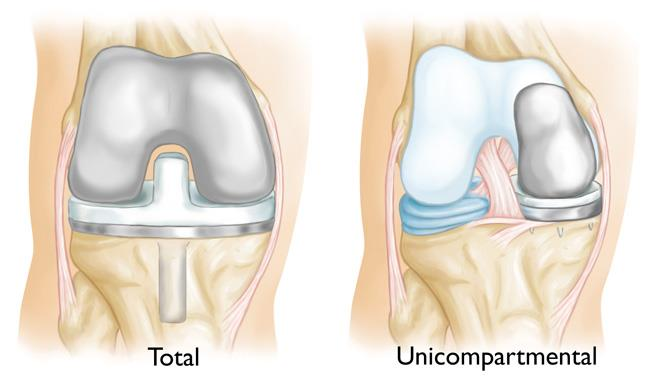
There are two types of knee replacements : Total Knee Replacement and Partial Knee Replacement. Partial Knee replacements are done by surgeons who are trained in the procedure. Most surgeons perform a total knee as a standard procedure for osteoarthritis whether it involves a single compartment or not. At Udai Omni, we perform partial or unicompartmental knee replacement if the arthritis is limited to one compartment. About 40% of our knee replacement procedures are partial. The benefits of partial knee replacement include:
- early recovery
- fewer complications like MI and DVT
- ability to sit on the floor and climb stairs
- natural feel of the joint rather than a feeling of a lump of metal in the knee
- ability to take part in leisure sports and activities
The success rate or survivorship of knee replacements in general are very good. Overall we are seeing a 90% survivorship at 20 years.
Many different types of implants are available. A standard implant made of cobalt chrome alloy and a polyethylene spacer is sufficient for over 90% of the patients. A ceramic coated implant like the “bionic gold” or “oxinium” prosthesis is advisable for those with allergy to artificial jewellery. There is no evidence that these implants perform better than a standard implant.
Hip Replacement:
The most common indication for a total hip replacement in India is Avascular necrosis of the femoral head. Other indications include rheumatoid arthritis, post traumatic arthritis, sequelae of childhood conditions like dysplasia, infections, Perthes’, SCFE etc.
Age is not a concern these days with advent of better materials and designs. Many patients in India tend to be young – in their 20s and 30s.
Floor activities: Traditionally, patients with hip replacements were told not to perform any activities on the floor. With better designs now available in India, a good competent surgeon should allow their patients to sit on the floor for various washroom activities and other activities like eating, praying etc. Many patients with a hip replacement get back to a normal lifestyle which can also include gentle sporting activities like badminton, table tennis, golf, trekking etc.
There are essentially two types of hip replacements – cemented and uncemented. Both perform equally well although the tendency is to do uncemented hips in the younger people. The bearing – ie the ball and the socket lining are the key for long term success. Ceramic heads and liners are generally recommended in the young and a metal head with polyethylene line may be suitable for the middle aged to elderly.
Survivorship and success of most standard hip replacements has improved significantly over the last few decades. Now, over 90% of our patients can expect their hip to survive 20 years. I would imagine this figure will get better as we follow our patients up in the future.
Enhanced Recovery after joint replacement:
Success of joint replacement, whether it is the hip or the knee depends on many factors. A well trained experienced surgeon is the key. However, other factors like patient engagement, physiotherapy and pain management are also extremely important.
At our hospital, we provide multi modal analgesia with the help of our expert anaesthetists to mobilise the patient within a day of surgery and discharge them home within 3 days on average. With advent of ambulatory selective nerve blocks and judicious use of oral and injectable analgesics, our patients mobile early and their VAS (visual analog score) for pain out of 10 is usually between 2-4. Knee and hip replacement need not be a painful experience any more.
The Future:
Surgery and joint replacement for advanced arthritis is going be around for a long time to come. There is no procedure or medicine to reverse advanced arthritic changes and deformity, whether it is the hip or the knee. No stem cell procedure or cartilage regenerative procedure will help in this regard. Media and pharmaceutical industry have a long track record of influencing the patient who would obviously prefer conservative procedures over surgery.
Industry is working on improving the performance of the implant by improving the coating and bearing materials.
Preventing arthritis by keeping oneself active and lean may be the best solution to prevent future arthritis and this avoid surgery.
Biological replacement from either ones own tissue or animal tissue is still a distant dream but a lot of work is being done across the world.